Chinook Regional Hospital in Lethbridge, photo credit Graham Ruttan
As fall approaches, COVID-19 continues to pose serious health and policy challenges for Canadians. While daily new infections are not as high as during the peak in May, they are up from a low in July. Recent daily new infections are estimated to be in the range of 500–1,000, as shown in Figure 1.
Figure 1: Daily New Infections in Canada
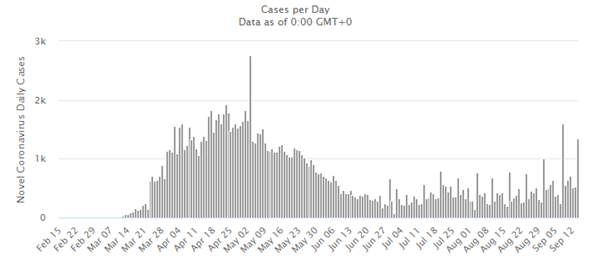
Source: Worldometers.com
With the risk of a strong second wave of infections this fall, potentially stretching medical systems, telehealth provision is a growing critical priority area. Some progress has already been made for enabling remote healthcare provision, but more can be done.
The private sector has also taken steps to facilitate the use of information technology in medical services. On Tuesday, Loblaws, through its subsidiary Shopper’s Drug Mart, signed a $75 million deal to obtain a minority stake in Toronto-based Telemedicine firm Maple.[1] Maple lets Canadians talk to doctors online in under two minutes. Patients can get advice, diagnosis, and treatment within the app, including digital sick notes, and prescriptions that are faxed to a local pharmacy. Telemedicine innovations like this provide Canadians with safer and more cost-effective medical services while minimizing the risk of spreading diseases, including (but not limited to) COVID-19.
The following is an excerpt from ICTC’s June 2020 report, Economic Resiliency in the Face of Adversity: From Surviving to Prospering. The report provides policymakers insights on steps that could be taken to ensure Canada emerges from the COVID-19 crisis in strong shape.
Section IV: Enabling a Resilient and Connected Health System
The novel coronavirus crisis has tested our healthcare system and caused considerable human suffering. However, the pandemic has also raised the opportunity to restructure our healthcare system for the better. In 2019, the World Bank estimated that Canada had fewer doctors per capita than the OECD average and fewer than Commonwealth nations like the United Kingdom and Australia. Indeed, Australia has about 38% more physicians per capita than Canada, whereas Sweden has more than double. While Canadians take great pride in their healthcare system relative to the United States, the US has almost the same number of physicians per capita.
Figure 2: Physicians per 1,000 Residents (Sample of OECD Nations, 2019)
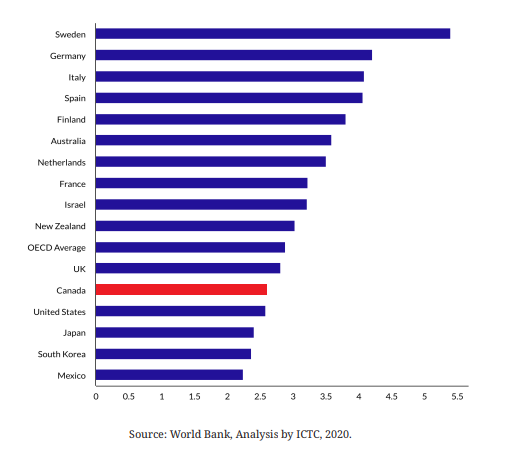
Although the number of Canadians graduating from medical schools each year has increased over the past decade, as Canadians age, the demand for doctors and healthcare services is expected to grow. Funding new medical schools in Canada or more seats in existing schools, raising hourly wages for doctors, or allowing nurses to provision more healthcare services are all obvious ways to increase the supply of critical medical professionals. While technology cannot create more physicians, recent developments have shown that it can make doctors more accessible.
COVID-19 has spurred innovation that until now has been impeded by policy hurdles. Telemedicine in recent years has represented just 0.15% of all billable services in the Canadian healthcare system,[2] but state-imposed quarantines during the health crisis have effectively forced the loosening of existing restrictions and allow the provision of this necessary service. In Ontario, for instance, the Ministry of Health announced in March that doctors could conduct patient visits by video or phone, which opens the door to widespread use of telemedicine for the first time.[3] While telemedicine was technologically feasible for a long time, COVID-19 provided the impetus to restructure policies that make it legal.
The benefits of telemedicine extend beyond patient services. It can be a critical instrument that helps prevent healthcare worker exposure to COVID-19 or other dangerous pathogens. Telemedicine can also help prevent patients from infecting one another, improve access for Canadians with disabilities or those living in remote communities or others who struggle to physically visit a doctor’s office or hospital. Waiting in one’s own bed as a “virtual waiting room” is surely safer and more comfortable than in a hospital room or doctor’s office waiting room, where the chance of contagion can be high. Canadian tech firms such as Vancouver-based Medeo Virtual Care, owned by QHR Technologies, are ready to meet the latent demand for such services. In the US, policies are also being loosened for telehealth[4] to make it more widely available and effective. Telemedicine’s time may have finally arrived — and strangely, on the heels of a global pandemic.
[1] The Canadian Press Staff, “Loblaw investing $75 million for minority stake in telemedicine firm Maple”, CTV News, September 15, 2020, https://www.ctvnews.ca/busines…
[2] “Virtual Care in Canada: Discussion Paper”, Canadian Medical Association, https://www.cma.ca/sites/defau… discussionpaper_v2EN.pdf.
[3] Avis Favaro, et al., “Ontario implements virtual medical visits in bid to keep doctors, patients safe amid COVID-19”, CTV News, March 14, 2020, https://www.ctvnews.ca/health/…
[4] Lev Facher, “Trump lifts restrictions on telehealth services for seniors in hopes of limiting coronavirus spread”, STAT, March 17, 2020, https:// www.statnews.com/2020…